Distal Clavicle Excision
What is a Mumford Distal Clavicle Excision?
A Mumford procedure or distal clavicle excision is a procedure performed for patients with arthritis at the acromioclavicular joint or distal clavicle osteolysis. The procedure is performed arthroscopically with removal of 5 to 6 mm of bone from the end of the clavicle to increase the space between the end of the collar bone and the opposite side of the joint (acromion). An open distal clavicle excision is also possible in cases of revision procedures or instability of the clavicle.
Anatomy
The shoulder is formed by three bones, humerus (upper arm bone), scapula (shoulder blade) and clavicle (collar bone). The head of the humerus fits into a cavity at the side of the scapula called the glenoid to form the glenohumeral joint. A projection of bone from the scapula called the acromion joins the outer end of the clavicle to form the acromioclavicular (AC) joint.
Causes of Degeneration of the AC Joint
The AC joint can undergo injury from trauma or degeneration due to osteoarthritis (breakdown or damage to the protective cartilage) because of aging, trauma, infection or joint instability. Similar to the meniscus of the knee, the cartilage disc of the joint degenerates by fraying, tearing, and forming holes, macerated by defects in the cartilage surface leading to arthritis. It is unclear how often these changes occur in asymptomatic patients, which can complicate diagnosis. Athletic use in can also cause damage to the joint through repetitive compression at the joint due to loading with heavy weight causing the blood supply at the end of the clavicle to become compromised. When the blood supply is compromised, it can lead to degeneration of the cartilage at the end of the clavicle called osteolysis.
Symptoms of Acromioclavicular Joint Arthritis
Common symptoms include pain with motion of the shoulder joint, most notable with overhead and cross-body motions. Pain is referred to the top of the shoulder and sometimes to the neck. Similar symptoms can present with neck problems or impingement so xrays and physical examination are needed to diagnosis the problem. Mechanical symptoms such as popping, catching, or grinding within the joint can be present as well.
Physical examination and Imaging to Diagnose AC joint problems
Because AC joint arthritis or osteolysis is often present with rotator cuff tears, labral tears or biceps injuries, a careful examination is needed to rule out symptoms. Tenderness localized to the joint is the most sensitive and specific tool to determine the problem. Pain with cross shoulder motion is also common localized to the top of the shoulder. There are other examination maneuvers including the O’Brien’s test that can be useful to diagnose the problem. Typically, plain xrays are all that are required to determine the presence or absence of AC joint arthritis or osteolysis although symptoms often do not correlate with the severity of xray findings. MRI can be useful to rule out other pathology in the shoulder. Also, edema on the MRI on both sides of the AC joint has been found to be predictive of a symptomatic joint.
Treatment
If the joint is asymptomatic even in the presence of xray findings and even in the presence of undergoing a surgical procedure for another part of the shoulder, the joint should be left alone. We evaluated a group of patients treated at the University of Utah for rotator cuff tears and determined the incidence of AC arthritis at the time of surgery, the percentage of times the AC joint was treated at the same time and the percentage of time further surgery was needed at the AC joint because it was left alone at surgery. In over 800 patients undergoing rotator cuff repair, only 5% had a distal clavicle excision at the same time. 12% of patients were noted to have significant arthritis at the time of surgery, so less than half of those with arthritis had a distal clavicle excision. At follow-up, only 1% of patients required further surgery on the AC joint. The most important factor regarding the need for further surgery was whether they had tenderness at the AC joint before surgery. Therefore, if you are tender at the AC joint, that is the primary indication to have it treated with a rotator cuff tear, not if there is arthritis or a spur at the joint on xrays. (Link to article on treatment of AC joint arthritis)
Nonoperative treatment
Initial conservative treatment includes rest, ice and anti-inflammatory medications. Physical therapy does not have a significant role in the treatment of disorders of this joint. If those measures do not improve the symptoms, a corticosteroid injection can be useful. Improvement can be seen in over 80% of patients with an injection and a single injection can be long lasting. If the symptoms return, a second or even third injection is reasonable but the long-term success of subsequent injections are not as good as the first.
Surgical Treatment
Surgical treatment of a symptomatic acromioclavicular joint typically includes a distal clavicle excision. This can be performed either open or arthroscopically. A majority of the time, an arthroscopic distal clavicle excision is performed. In cases of failed arthroscopic excision, an open revision is reasonable or if there is deformity or hypertrophy at the distal clavicle that would limit the ability to perform an adequate resection arthroscopically.
The arthroscopic procedure uses three small portal sites that allow access to the joint for a camera and small burr. The burr is then used to remove approximately 5 mm of the end of the clavicle. Other procedures to the biceps or rotator cuff can be performed at the same time. Similarly, all other structures are evaluated visually during a distal clavicle excision. An open distal clavicle excision is performed through a small incision on the top of the shoulder. The muscles and ligaments are peeled off the clavicle, a saw is used to remove 5 mm of the end of the clavicle and then the ligaments are repaired. In the arthroscopic procedure, no ligaments are violated and therefore do not have to heal.
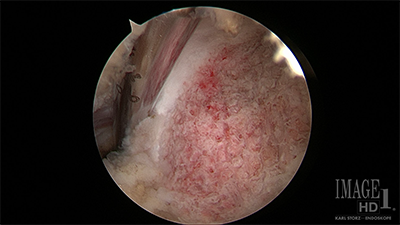
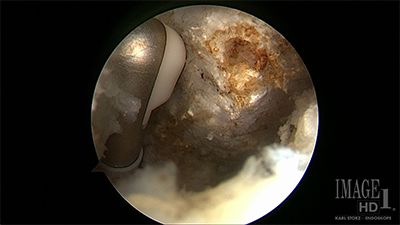
Figure - Arthroscopic view of the distal clavicle on the left before resection with an instrument inside the joint. Arthroscopic view of the distal clavicle on the right after resection with an instrument in the joint showing an adequate resection.
Postoperative Course
Surgery is typically outpatient where patients will come in and go home the same day. They will be treated postoperatively with an interscalene cathether placed under ultrasound by our anesthesia pain specialists as well as oral medication. If an isolated arthroscopic distal clavicle excision is performed, the dressings can be removed in 3 days and the patient has a sling for comfort which they can remove that night. They can be using the arm for everyday activities including lifting up to 10 lbs. At 2 weeks, therapy will be initiated at home and with a therapist. At 6 weeks, patients will be allowed to return to all activities. If another procedure is performed at the same time, then the postoperative restrictions are based upon the restrictions of the other procedure.
In the setting of an open distal clavicle excision, the patient will have to wear a sling for 3 weeks daytime and nighttime. The dressings may be removed between 5 days after the procedure and the wounds can get wet in the shower at that time. Patients will take the sling off, let the arm to the side in the shower, let the water run over wounds without soaping or scrubbing and then pat dry the shoulder and place the sling back on. Washing under the armpit is allowed. For the first 2 weeks, patients will be doing only elbow wrist and hand range of motion. At 2 weeks, the sutures will be removed from the wounds and patients will start physical therapy. At 3 weeks, patients may discontinue the sling and start using the arm for everyday activities with no lifting over 10 lbs. Stretching with therapy will continue. At 8 weeks, strengthening with therapy will start and the patient may lift up to 30 lbs. At 3 months, the patient will be able to return to all activities without restrictions.
You will need the Adobe Reader to view and print these documents.






