Distal Triceps Tendon Ruptures and Repair
Acute ruptures of the distal triceps tendon are a relatively rare injury. These injuries generally occur in middle aged men after forceful elbow extension. Triceps tendon rupture is more frequent in those between 30 and 50 years of age, and is twice as frequent in males. In general, tears of >50% of the tendon insertion are treated surgically. Various repair methods have been described in the literature with the aim of restoring the normal tendon footprint insertion. These repair methods include use of transosseous bone tunnels with nonabsorbable suture.
Anatomy
The triceps muscle, as indicated by its name, includes three heads. The long head originates from the scapula, while the medial and lateral heads originate from the humerus. These three heads join together at elbow level and attach to the olecranon to form one of the strongest tendons in the body. It covers the whole back of the arm, and its rupture is very rare. In general, a triceps rupture occurs as a detachment of tendon from the bone. Musculotendinous junction or intramuscular ruptures are very rare. The attachment of the triceps tendon to the olecranon has been shown to be spread over a large area.The footprint was described as dome-shaped.
Etiology
Triceps tendon rupture results from overloading on the extended elbow, or an abrupt contraction of the muscle. The most frequent mechanism in the literature is a fall on the hand with the elbow in extension. Weightlifting is a high-risk athletic activity for triceps rupture. Risk of triceps rupture is especially high in weightlifters and body building athletes, in part due to the potential use of anabolic steroids. The potential for triceps rupture is higher in patients with diseases affecting collagen. These diseases include chronic renal insufficiency requiring dialysis, rheumatoid arthritis, systemic lupus erythematosus (SLE), diabetes, Marfan’s syndrome, osteogenesis imperfecta, and metabolic bone diseases leading to hyperparathyroidism. Chronic olecranon bursitis increases the risk of triceps tendon rupture since it causes chronic inflammation around the tendon.
Diagnosis
Patients often describe a pop at the detachment site on the back of the elbow. Swelling and bruising are frequently seen at the back of the elbow. A gap can be felt at the tip of the forearm bone where the tendon inserts. Although a significant reduction in extension strength is normally present, complete loss of active extension is seen in only 20% of cases. The presence of an intact lateral expansion of the tendon may allow active extension even in complete rupture. This may lead to misdiagnosis, or delayed diagnosis of the rupture.
Xrays are typically normal although there can be a fleck of bone where a small avulsion occurs with the tendon off the bone. MRI is diagnostic for a rupture showing detachment of the tendon from the bone. (Figure 1)
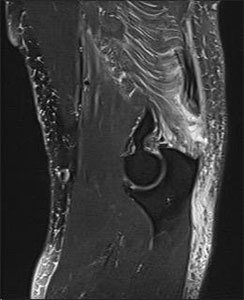
Figure 1 – MRI showing avulsion of the triceps tendon off the proximal ulna
Treatment
Most complete triceps tendon ruptures require repair otherwise there will be a significant loss of extension strength. Full tears should be repaired within 2 to 3 weeks of injury otherwise these may need to be augmented with a graft to obtain a complete repair. Partial tears less than 50% of the width of the insertion may be considered for nonoperative treatment although over 50% of these patients will fail nonoperative treatment due to persistent pain and weakness and go on to surgical repair.
Surgery is performed typically in an outpatient setting. Dr. Tashjian will repair distal triceps tendon ruptures using high strength suture and crossing bone tunnels. (Figures 2 through 4) He has previously reported on his surgical results of his patients with excellent long-term outcomes after distal triceps tendon repairs using bone tunnels. (Tashjian's Distal Triceps Tendon Repair Manuscript)
Postoperatively patients are treated with an interscalene nerve block for pain control. They are splinted in full extension for a week and then progressively perform range of motion limited to 90 degrees of elbow flexion for the first 6 weeks after surgery protected by a sling between therapy sessions. At 6 weeks, the sling is discontinued. The patient continues to regain full motion until 12 weeks. At 12 weeks postoperative, strengthening is started with plans for full return to activity by 6 months postoperative. Recovery is expected to be complete with full return of strength and sporting activities including weight lifting.

Figure 2 – Distal triceps tendon avulsion off the ulna
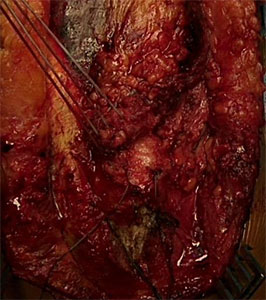
Figure 3 – Heavy nonabsorbable suture passed into the triceps tendon for repair

Figure 4 – Sutures passed through bone tunnels in the ulna and tied completing the repair
You will need the Adobe Reader to view and print these documents.






