Shoulder Instability and Labral Repair
Shoulder Instability
The glenohumeral joint of the shoulder, or the “ball and socket” joint, is purposely built to allow a wide range of motion while maintaining a stable relationship between the ball (humerus) and the socket (glenoid). The critical aspect of the shoulder is a balance between stability and motion. There are several structures that provide stability and failure of one or more of these restraints can lead to abnormal motion or instability.
There are several types of instability but in general instability is commonly grouped based upon the direction the humerus dislocates or moves more than it is supposed to (subluxates). The common directions are anterior (forward), posterior (backwards) or multidirectional (front, back and bottom). The typical position of the arm in which that the shoulder dislocates determines the direction. The most common type of shoulder instability is anterior (>80%) and this occurs with the arm overhead in a position as if you were throwing a ball. Typically, the arm is pulled back in the position and the humerus moves forward on the glenoid. This injury most commonly occurs with falls especially while playing sports. Posterior instability is less common and occurs in the setting when the arm is across the chest as if you are reaching to scratch the outside of your opposite shoulder and a blow occurs to the elbow driving the humerus backwards. This typically occurs in specific sports injuries including football lineman. It can also result due to severe contraction of the muscles around the shoulder instead of a direct blow as seen with seizures or electrocutions. Multidirectional instability (MDI) is relatively uncommon. The two settings MDI occur in are young, healthy flexible women usually under the age of 20. They are loose jointed and can usually hyperextend their fingers or elbow and can touch the floor with their palms. The complaint is most often pain instead of full dislocations although can also complain of subluxations. Complaints typically occur with carrying heavy bags or suitcases where the shoulder feels to be pulling out the bottom. The other group of patients with MDI are patients with a collagen tissue disorder like Ehlers Danlos Syndrome or Marfan’s Disease. These patients have more profound instability symptoms in all directions that can even include full dislocations. The key aspect of the MDI diagnosis is there is no specific trauma or injury that leads to the symptoms.
Laxity Versus Instability
The first thing that needs discussion with instability is defining the terms we use to speak about it. We must differentiate laxity versus instability. Laxity is normal translation of the humeral head that is symptom free and causes no pain. There is a wide variation of laxity between people with the key being this is normal for each individual. Instability is an abnormal condition with pain or discomfort with the feelings of abnormal motion due to excessive translation of the humeral head on the glenoid with active motion. The diagnosis and treatment described below is for patients with shoulder instability, not laxity.
Stabilizers of the Shoulder
The structures of the shoulder that provide stability include the shape of the bones (humerus and glenoid) and whether loss of bone has occurred, the ligaments in the front and back of the joint, the rotator cuff muscles surrounding the joint and the labrum. The ligaments of the shoulder run from the ball of the humerus and insert onto the glenoid socket edge. The attachment onto the glenoid is a ring of fibrocartilage that surrounds the socket like a gasket. This ring connects the ligaments to the glenoid and is called the labrum. If the shoulder dislocates, the ring of cartilage is typically ripped off the edge of the glenoid with the ligaments in either the front (anterior dislocation) or the back (posterior dislocation) of the shoulder and the ligaments are stretched. During an arthroscopic instability repair or stabilization procedure, the ligaments are typically restored back to the glenoid with tightening or shortening of the ligaments.
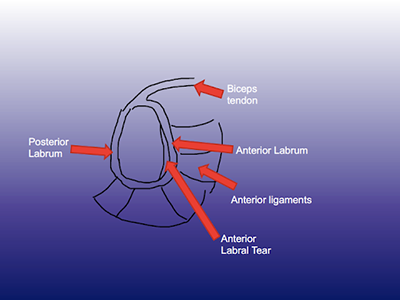
After a dislocation, a labral tear, or sometimes called a Bankart lesion, occurs in up to 90% of cases. When the shoulder comes out of the socket, the round humeral head lodges on the glenoid creating an impression or dimple. The dimple is called a Hill-Sachs lesion and occurs between %60 to 90% of dislocations. Often times the Hill-Sachs is small and can be left alone. Occasionally it is large and needs to be treated during surgery often with filling the defect with soft tissue from the rotator cuff (reimplissage). About 50% patients with repetitive dislocations out the front of the shoulder will have some chipping of the bone off the front, like chipping of a golf tee. This injury is often not significant and can be ignored. In larger injurys (greater than 13% of the width of the glenoid), the surgical procedure often needs to be altered by including other arthroscopic methods of stabilization (reimplissage) or using an open soft tissue repair (Bankart repair) or bone transfer procedure (coracoid transfer [Latarjet] or allograft [distal tibia]). The most common surgical procedure for recurrent instability is an arthroscopic labral repair where anchors are placed into the edge of the glenoid and sutures from these anchors are passed around the labrum and into the ligaments to repair them back to the position where they detached from.
Symptoms of Shoulder Instability
Patients with instability will often present with pain in the front or back of the shoulder, especially when the shoulder dislocates. With anterior instability, patients after often pain free between episodes of instability but will feel apprehension or the feelings the shoulder will dislocate when the arm is positioned overhead. With posterior instability, full dislocations are uncommon rather the most common symptom is pain with bringing the arm across the body. Locking or catching can occur as a result of fragments of the labrum in the shoulder. Reduced range of motion is also possible over time as a result of avoiding certain ranges due to feelings the shoulder will dislocate.
Diagnosis
The diagnosis of shoulder instability is often based upon history and physical examination. The history will include a traumatic event that leads to the shoulder needing to be reduced or the patient self-reducing the shoulder with traction. Physical examination by a physician will confirm the diagnosis and direction using maneuvers that make the feelings of instability worse and then better.
X-rays, computed tomography (CT) scan or magnetic resonance imaging (MRI) scan, with an intraarticular contrast medium, may be ordered to determine the presence of labral tears or bone injury. MRI will confirm detachment of the labrum in either the front or back of the shoulder. A CT scan can be ordered to determine the extent of bone loss on the humerus and glenoid. 3D reconstructions of the humerus and glenoid are typically performed in order to quantify bone loss as these measures will often drive the type of surgical procedure required if surgery is indicated.
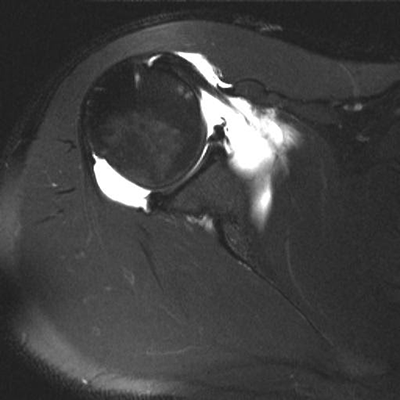
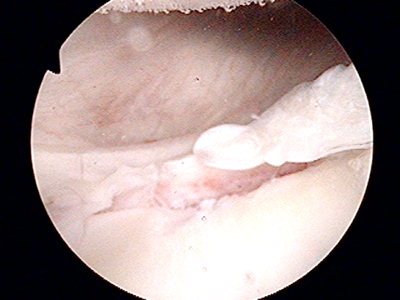
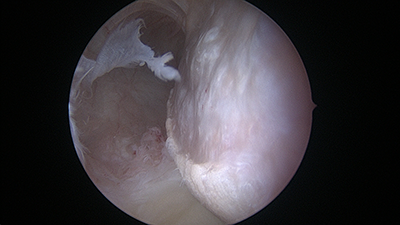
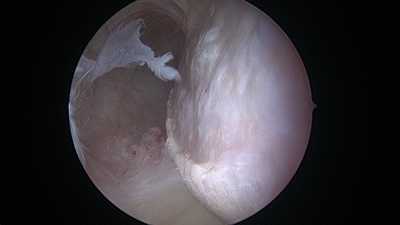
Anterior labral tear (arrow) on MR arthrogram after anterior dislocation corresponding to the labral tear identified during arthroscopic labral repair (arrowhead)
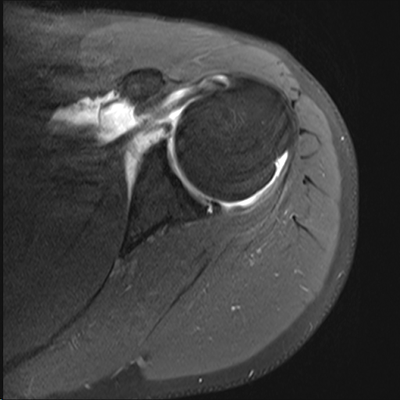
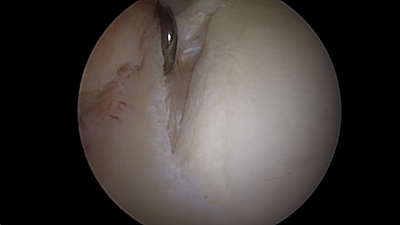
Posterior labral tear (arrow) on MR arthrogram after posterior shoulder dislocation corresponding to the posterior labral tear identified during arthroscopic labral repair (arrowhead)

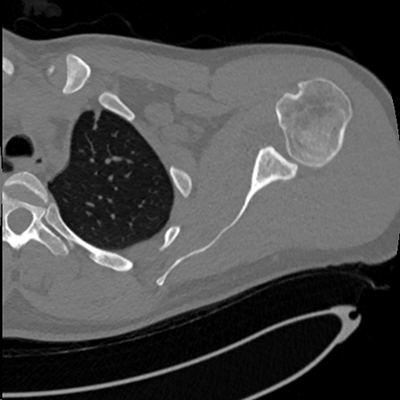
3D reconstructed CT scan and 2D CT scan of a patient with anterior glenoid bone loss on the 3D image (arrow) and 2D image (arrowhead)
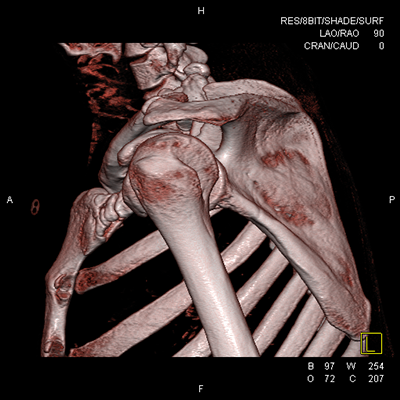
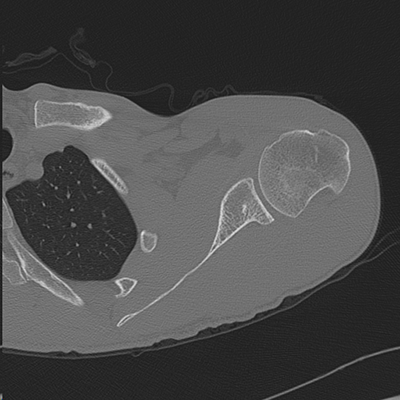
3D and 2D CT scan showing large Hill-Sachs deformity of the humeral head associated with anterior instability (arrow) and arthroscopic view (triangle) corresponding to the Hill-Sachs lesion
Treatment
Treatment of an acutely dislocated shoulder includes closed reduction. Closed reduction often required sedation although an injection of anesthetic into the joint can aide the reduction and often does not require sedation. Once the joint is reduced, acute management includes the use of sling for a period of time until the shoulder starts to feel more comfortable. There is no data to support that position of immobilization matters therefore a simple sling all that is required. Length of sling wear depends on the chances for the sling to prevent recurrence of instability. In the cases of no significant injury to the bone with just a labral injury after a first-time dislocation, the primary risk factor for recurrence is the age of the patient. The risk for recurrence after a first-time anterior dislocation is based on the age range of the patient: age 12 to 22 – 72% recur; age 23 to 29 – 55% recur; age 30 to 33 – 30% recur; age 34 to 40 – 20% recur. There is some limited information that would support 3 weeks of sling wear may assist with reduction in recurrence. Other factors associated with recurrence include significant bone injury on the humeral head or glenoid, contact or collision sports, hyperlaxity, duration of time from the dislocation.
In the setting of anterior labral tearing or anterior instability, the decision to undergo continued nonoperative treatment versus undergoing surgical repair after a first dislocation is primarily dependent on the chances for recurrence based upon the factors previously described as well as the consequences of a second dislocation if it occurs. In general, patients over the age of 30 should be guided towards initial nonoperative treatment as the risk for recurrence in this age group is less than 30% and the re-dislocation rates after arthroscopic instability repair are approximately 10% so the expected value of surgery does not exceed that of nonoperative treatment. If a patient has a second dislocation, the chances for a third are 100% if activity is not modified therefore any patient is indicated for surgical repair after a 2nd dislocation. There is a 90% return to play or sport with repair after a single dislocation as well as a 2nd dislocation and there is no increase in re-dislocation rate after arthroscopic repair after 1 or 2 dislocations, therefore this strategy does not impact outcomes in this age group. In patients under the age of 30, the risk of recurrence is much higher and therefore the risk of re-dislocating without surgery should be taken in context of the risk of re-dislocating after surgery (10%). In young, high demand patients who can’t afford a second dislocation such as an in season or preseason dislocation, then surgery after a single dislocation can be considered and will be discussed.
In the setting of posterior labral tearing or posterior dislocations do not recur commonly unless there are very large bone defects. Typically, posterior dislocations will undergo rehabilitation first for at least 6 weeks including range of motion exercises, posterior rotator cuff (infraspinatus and teres minor) and posterior deltoid strengthening along with scapular stabilizer strengthening. If patients fail a course of nonoperative treatment and they still have pain primarily, then undergoing a posterior labral repair is indicated.
Surgical Treatment of Shoulder Instability
A majority of patients can be treated with an arthroscopic repair for recurrent instability of the shoulder, either anterior or posterior. The surgery is typically outpatient where patients will come in and go home the same day. The surgery is done using small instruments and cameras. Small anchors which look like screws are inserted into the edge of the glenoid where the labrum was detached. There is an eyelet at the top of the anchor where string or suture is held. The suture is then passed around the labrum and tied to complete the repair. Repair can be performed of both the anterior and posterior labrum arthroscopically. In cases of large Hill-Sachs lesions on the humerus, a reimplissage procedure is performed arthroscopically repairing soft tissue into the humeral head defect.
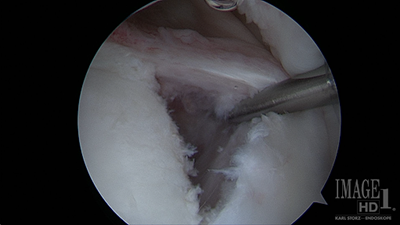
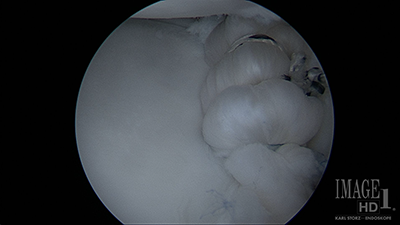
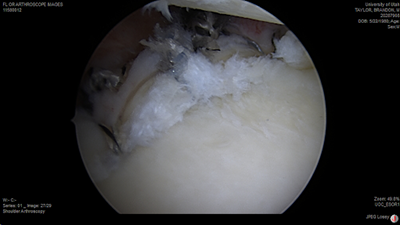
Arthroscopic view from above with a labral tear being pulled from the glenoid before repair (left) and after repair of the labrum back to the glenoid (right)
Posterior labral tear (left image) prior to repair and after arthroscopic repair (right)

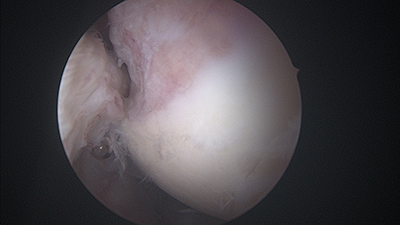
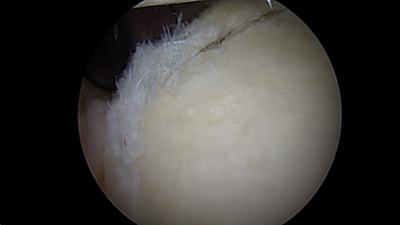
Arthroscopic view of a large Hill-Sachs lesion (left), after anchors have been placed for reimplissage procedure (middle) and final view of repaired tissue into the Hill-Sachs defect (right)
In cases of larger injuries to the bone, either a Latarjet procedure (coracoid transfer) or an allograft (distal tibial) reconstruction of the glenoid will be performed or an allograft reconstruction of a very large Hill-Sachs defect can be performed. Typically, a Latarjet procedure is reserved for patients with glenoid bone loss over 20% of the width of the glenoid surface. A distal tibial allograft is reserved for patients that have over a 30% defect of the width of the glenoid width or in revision settings of a failed Latarjet. An open soft tissue Bankart procedure is typically reserved for patients with greater than 13% to 20% glenoid bone loss but without a significant Hill-Sachs lesion.

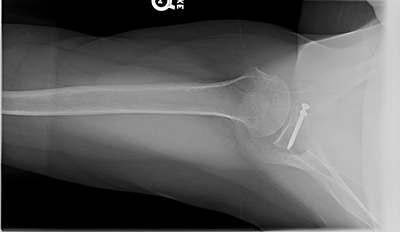

3D CT scan shows 25% anterior glenoid bone loss; Postoperative xrays after Latarjet procedure showing healing glenoid graft and restoration of the anterior glenoid bone
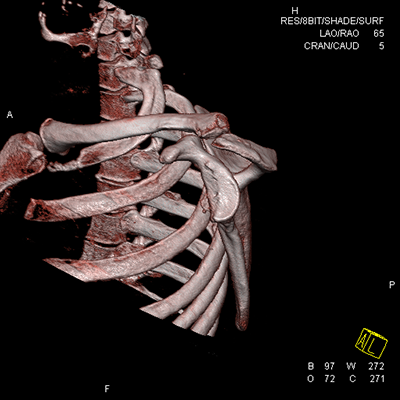

3D CT scan showing 40% anterior glenoid bone loss; Intraoperative view of glenoid with anterior glenoid rim defect (triangle)


Distal tibial allograft after shaping for the defect; Final reconstruction of anterior glenoid using two screws to fix the distal tibial allograft
Postoperative Treatment after Arthroscopic or Open Instability Repairs
Surgery is typically outpatient as patients will come in and go home the same day. Patients will be treated postoperatively with an interscalene cathether placed under ultrasound by our anesthesia pain specialists as well as oral medication. Patients will be in a sling for 6 weeks during the daytime and nighttime. The dressings may be removed between 3 to 5 days depending on the extent of the procedure and the wounds can get wet in the shower at that time. Patients will take the sling off, let the arm to the side in the shower, let the water run over wounds without soaping or scrubbing and then pat dry the shoulder and place the sling back on. Washing under the armpit is allowed. For the first 2 weeks, patients will be doing only elbow wrist and hand range of motion. At 2 weeks, the sutures will be removed from the wounds and patients will start physical therapy. At 6 weeks, patients may discontinue the sling and start using the arm for everyday activities with no lifting over 5 lbs. Stretching with therapy will continue avoiding the position at risk for the surgery (anterior instability – throwing position avoided; posterior instability – bringing the arm across the midline or behind the back will be avoided). At 10 weeks isometric strengthening is started. At 12 weeks, resistive strengthening with therapy will start and the patient may lift up to 20 lbs. At 4.5 months, the patient will be able to lift up to 40 lbs and at 6 months return to all activities. There will be continued improvement in range of motion and strengthening for up to 12 months after surgery. Return to sport includes walking on the first postoperative day and stationary bike at 2 weeks. Running and jogging can start at 6 weeks. Swimming in a pool and road cycling can start at 3 months. Golf and tennis can start at 4 months. All other contact sports (downhill mountain biking, climbing, contact or collision sport) may be initiated at 6 months postoperative.





