Distal Biceps Tendon Rupture Repair and Reconstruction
Distal Biceps Tendon Ruptures and Repair
Rupture of the distal bicep tendon is a relatively uncommon injury that may have important consequences regarding the strength and function of the arm. Most of these occur in the dominant extremity of male patients between the ages of thirty and sixty years. About 1 distal biceps tendon rupture occurs for every 100,000 patients per year with the average age in the late forties. Almost 90% of cases occur in the dominant arm. In general, most complete distal biceps tendon ruptures are recommended to be repaired as they will leave the patient with a strength deficit. Partial thickness tears can be treated nonoperatively although many of these will still remain painful and subsequently require surgical repair. (Tashjian's Distal Bicep Tendon Rupture Review Manuscript)
Anatomy
The biceps muscle has two tendinous origins and one tendinous insertion. The long head of biceps originates at the supraglenoid tubercle and traverses the shoulder joint prior to exiting through the lateral rotator cuff interval. It then passes through the intertubercular groove into the proximal arm. The short head takes origin from the coracoid. There are two bones of the forearm, the radius and ulna. The distal biceps tendon inserts onto the radius into the radial tuberosity and primarily functions to turn the forearm up and assist with elbow flexion. The radial tuberosity has a footprint for tendon insertion. The tendon footprint measures 19 mm proximal to distal and 4 mm medial to lateral. The long head distal tendon was noted to be crescentic, deep and insert proximally on the tuberosity, while the short head distal tendon was consistently oval, superficial and inserted distally on the tuberosity. About 50% of the strength required to turn the forearm up is provided by the biceps and about 20% of elbow flexion strength is provided by the biceps.
Etiology
The etiology of distal biceps tendon ruptures is not well understood but probably most likely due to limited vascularity of the tendon and trauma. There is limited vascularity a few inches from the insertion onto the radius bone. Also, with rotation the space available for the tendon narrows which may also predispose towards injury and impingement.
Symptoms
Patients with an acute distal bicep tendon rupture will have immediate onset pain and weakness. Often there is a pop in the arm that then leads to bruising. There is often deformity as well with the biceps muscle belly rising up in the arm as it has lost it attachment to the forearm. With time the bruising and pain will go away often in a few days to week and then the patient will just be left with a loss of strength. There is often not a significant amount of pain with complete distal biceps tendon ruptures but there is a significant loss of strength. Partial distal bicep tendon ruptures with some remaining tendon attached to the radius will often present with pain primarily and not weakness. Symptoms are often provoked by forearm rotation like turning a screwdriver.
Physical Examination and Imaging
Physical examination for a distal bicep tendon rupture is relatively simple. Often patients will have full range of motion and no loss of stability. There will be deformity of the muscle with rising up of the belly in the forearm. With passive rotation of the forearm, there will be no movement of the belly of the muscle. Also, a positive hook test is almost 100% sensitive to pick up the problem. The opposite finger can hook the tendon in the normal state but there is nothing to hook in the injured state. A painful hook test but with an intact structure is often diagnostic for a partial tear. Xrays are typically normal but an MRI is diagnostic showing a torn retracted tendon from the insertion. (Figure 1 and 2)
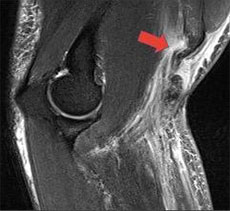
Figure 1 ‐ MRI showing torn distal bicep tendon (arrow)
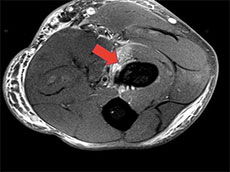
Figure 2 ‐ MRI showing footprint on radius with absent distal biceps tendon due to rupture (arrow)
Treatment
Most patients will electively decide to undergo distal biceps tendon repair otherwise they will lose 50% of their rotation power of their forearm and 20% of their elbow flexion strength. Lower demand patients in the nondominant extremity may decide to treat this without repair. It will not heal on its own and while it is unlikely to cause any pain it will cause weakness.
Optimal timing for surgery is within the first 2 weeks of injury. Primary repair can be performed up until 6 weeks from injury. Beyond 6 weeks, patients will often need augmentation of the tendon with a graft (allograft) to extend the tendon in order to complete a repair.
Dr. Tashjian will perform the procedure as an outpatient. Dr. Tashjian does the surgery through a single incision on the front of the forearm. The tendon is mobilized and then 3 sutures or stitches of high strength suture are passed in a locking fashion into the tendon. The sutures are then passed into two anchors which are then placed into the radius. (Figure 3) The sutures are tied completing the repair.

Figure 3 – Xray of elbow with 2 suture anchor repair of the distal biceps tendon
Postoperatively patients are treated with an interscalene nerve block for pain control and are placed into a sling and a splint. The splint is removed at 1 week and elbow range of motion is started but the patient comes in and out of the sling for the next 5 weeks protecting the elbow between therapy sessions with the sling. At 6 weeks postoperative, the sling is removed. The patient can start to lift up to 5 lbs at 6 weeks. At 3 months, 20 lbs of lifting is allowed as well as return to road biking and swimming. At 4.5 months, 40 lbs of lifting is allowed and return to most activity except high demand sport and contact or collision sport. At 6 months, the patient can return to all activity.
In cases of delay, a distal biceps tendon reconstruction can be performed by Dr. Tashjian. These are cases where there is insufficient tendon left due to delay. (Figure 4) Dr. Tashjian performs the reconstruction either using a hamstring allograft tendon (see below – Figure 5) or Achilles allograft tendon. The allograft is weaved into the native tendon and then the graft is repaired down to the radius using the same technique as a primary repair. The postoperative rehabilitation is the same as a primary repair and the outcomes are similar.
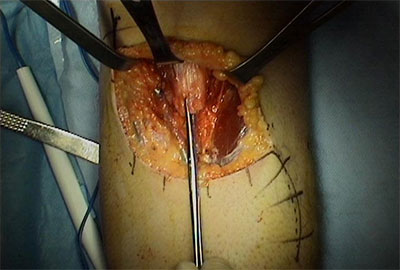
Figure 4 – Remnant of the distal bicep tendon after rupture limiting repair
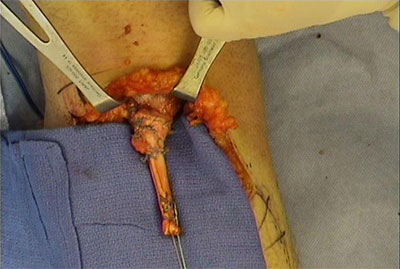
Figure 5 – Hamstring allograft tendon extension of the distal biceps muscle creating a new distal bicep tendon for repair using suture anchors and a similar technique as a primary repair
You will need the Adobe Reader to view and print these documents.






